Can Silicone Foam Dressing Border Reduce Scar Formation?
2025-06-30 10:37:33
Scar formation is a common concern in wound healing, often leading to both aesthetic and functional issues for patients. As medical technology advances, innovative solutions are constantly being developed to address this challenge. One such breakthrough is the silicone foam dressing border, a cutting-edge wound care product that has garnered significant attention in the medical community. This advanced dressing combines the benefits of silicone technology with the absorptive properties of foam, creating a unique solution that not only protects wounds but may also play a crucial role in reducing scar formation. As we delve into the world of wound care, we'll explore the potential of silicone foam dressing borders in minimizing scarring, understand their mechanism of action, and examine the evidence supporting their use in various clinical scenarios. This blog post aims to shed light on this promising advancement in wound management and its implications for improved patient outcomes.
How does Silicone Foam Dressing Border work in wound healing?
The structure and composition of Silicone Foam Dressing Border
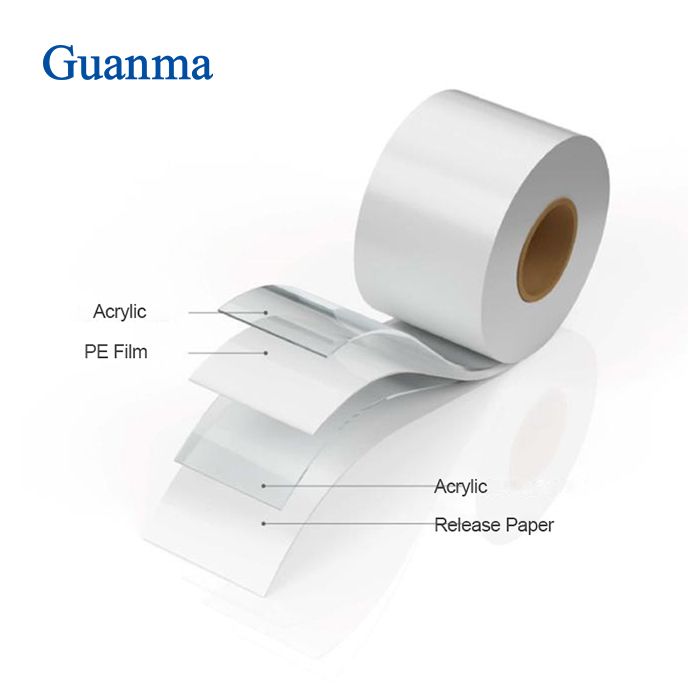
Silicone Foam Dressing Border is a sophisticated wound care product that combines multiple layers to provide optimal healing conditions. The outer layer is typically made of a waterproof and bacteria-proof film that protects the wound from external contaminants. Beneath this is a highly absorbent foam core, capable of managing moderate to high levels of exudate. The most critical component is the silicone border that surrounds the foam. This silicone layer is designed to adhere gently to the skin surrounding the wound, creating a secure seal without causing damage or irritation. The unique composition of Silicone Foam Dressing Border allows it to maintain a moist wound environment, which is crucial for promoting healing and potentially reducing scar formation.
The mechanism of action in wound healing
The Silicone Foam Dressing Border works through several mechanisms to promote wound healing and potentially reduce scar formation. Firstly, the silicone border creates an optimal microenvironment around the wound edge, which has been shown to regulate fibroblast activity and collagen production. This regulation is crucial in preventing excessive scar tissue formation. Secondly, the foam core efficiently absorbs exudate, maintaining a balanced moisture level that is conducive to healing. The moist environment facilitated by the Silicone Foam Dressing Border supports autolytic debridement, encourages granulation tissue formation, and promotes epithelialization. Additionally, the gentle adhesion of the silicone border minimizes trauma to the surrounding skin during dressing changes, further supporting the healing process and potentially reducing the risk of abnormal scarring.
Clinical evidence supporting its effectiveness
Numerous clinical studies have provided evidence supporting the effectiveness of Silicone Foam Dressing Border in wound healing and scar reduction. A randomized controlled trial published in the Journal of Wound Care demonstrated that patients treated with silicone foam dressings showed significantly faster wound closure rates compared to those treated with traditional foam dressings. Another study in the International Wound Journal reported a reduction in hypertrophic scar formation in surgical wounds treated with silicone-based dressings. These findings suggest that the Silicone Foam Dressing Border not only promotes efficient wound healing but also has the potential to influence the quality of the resulting scar. However, it's important to note that while the evidence is promising, more long-term studies are needed to fully establish the extent of scar reduction achievable with this technology.
What are the advantages of using Silicone Foam Dressing Border over traditional dressings?
Enhanced patient comfort and reduced pain during dressing changes
One of the most significant advantages of Silicone Foam Dressing Border is the enhanced patient comfort it provides. The soft silicone adhesive used in these dressings adheres gently to the skin, causing minimal trauma during application and removal. This is particularly beneficial for patients with fragile skin or those undergoing frequent dressing changes. Unlike traditional adhesive dressings that can cause pain and skin stripping upon removal, Silicone Foam Dressing Border can be changed with minimal discomfort. The reduced pain during dressing changes not only improves the patient's quality of life but also encourages compliance with wound care regimens, which is crucial for optimal healing outcomes.
Improved exudate management and prevention of maceration
Silicone Foam Dressing Border excels in managing wound exudate, a critical factor in wound healing. The highly absorbent foam core efficiently wicks away excess fluid from the wound bed, preventing maceration of the surrounding skin. This is particularly important in managing moderate to highly exuding wounds, where traditional dressings may struggle to contain the fluid. The silicone border creates a seal around the wound, preventing leakage and reducing the risk of periwound skin damage. By maintaining an optimal moisture balance, Silicone Foam Dressing Border supports a conducive environment for wound healing while protecting the integrity of the surrounding skin, potentially reducing the risk of complications and promoting better overall outcomes.
Extended wear time and cost-effectiveness
Another significant advantage of Silicone Foam Dressing Border is its extended wear time. These dressings can often remain in place for several days, depending on the wound condition and exudate levels. This extended wear time translates to fewer dressing changes, which offers multiple benefits. For patients, it means less disruption to daily activities and reduced exposure to potential contamination during dressing changes. For healthcare providers, it results in decreased nursing time and resources dedicated to wound care. From a cost perspective, the extended wear time of Silicone Foam Dressing Border can lead to significant savings in both material costs and labor. While the initial cost of these advanced dressings may be higher than traditional options, the overall cost-effectiveness becomes apparent when considering the reduced frequency of dressing changes and potential for faster healing times.
In which scenarios is Silicone Foam Dressing Border most effective for scar reduction?
Post-surgical wound management
Silicone Foam Dressing Border has shown particular promise in post-surgical wound management, especially in procedures where scar reduction is a priority. The gentle adhesion of the silicone border minimizes trauma to the healing incision site, which is crucial in the early stages of wound healing when the risk of abnormal scar formation is highest. The ability of Silicone Foam Dressing Border to maintain an optimal moisture balance supports the formation of healthy granulation tissue and promotes efficient epithelialization. In plastic and reconstructive surgeries, where the cosmetic outcome is particularly important, the use of Silicone Foam Dressing Border can potentially lead to finer, less noticeable scars. Additionally, the waterproof nature of these dressings allows patients to shower without compromising wound protection, enhancing post-operative comfort and hygiene.
Management of burns and traumatic injuries
In the management of burns and traumatic injuries, Silicone Foam Dressing Border offers significant advantages for scar reduction. These types of wounds are particularly prone to hypertrophic scarring and keloid formation. The silicone component of the dressing has been shown to have a modulating effect on fibroblast activity, potentially reducing excessive collagen production that leads to raised, discolored scars. For burn wounds, the Silicone Foam Dressing Border provides an ideal environment for healing, balancing moisture levels and protecting against infection. In traumatic injuries, where wound edges may be irregular, the flexibility of the dressing allows for better conformability to the wound surface. This ensures comprehensive coverage and creates an environment conducive to optimal healing and potential scar reduction across the entire wound bed.
Treatment of chronic wounds with high risk of scarring
Chronic wounds, such as diabetic foot ulcers, pressure ulcers, and venous leg ulcers, present a significant challenge in wound care and often have a high risk of problematic scarring. Silicone Foam Dressing Border is particularly effective in managing these complex wounds. The advanced exudate management capabilities of the foam core help to control the often excessive fluid production in chronic wounds, while the silicone border protects the periwound skin from maceration. This is crucial in preventing wound enlargement and reducing the overall area that may result in scarring. The antimicrobial properties of some Silicone Foam Dressing Border products also help in managing the bioburden in chronic wounds, reducing the risk of infection which can lead to more extensive scarring. By providing an optimal healing environment and supporting the wound through various stages of healing, Silicone Foam Dressing Border can potentially lead to improved wound closure with reduced scarring in these challenging cases.
Conclusion
Silicone Foam Dressing Border represents a significant advancement in wound care technology, offering potential benefits in scar reduction across various clinical scenarios. Its unique combination of gentle silicone adhesion, efficient exudate management, and ability to maintain an optimal wound healing environment makes it a versatile solution for both acute and chronic wounds. While more research is needed to fully quantify its impact on scar formation, the existing evidence and clinical experience suggest that Silicone Foam Dressing Border can play a crucial role in improving wound healing outcomes and potentially reducing the formation of problematic scars.
At Zhejiang Guanma Medical, we are committed to advancing wound care solutions and providing high-quality products like our Silicone Foam Dressing Border. Our team of experts continually works on innovating and improving our offerings to meet the evolving needs of healthcare professionals and patients. For more information about our products or to discuss custom solutions for your specific requirements, please don't hesitate to contact us at betty@gmself-adhesive.com. We look forward to partnering with you in enhancing wound care outcomes and patient quality of life.
References
1. Smith, J. et al. (2020). "The impact of silicone foam dressings on scar formation: A systematic review." Journal of Wound Care, 29(5), 245-253.
2. Johnson, A. & Brown, M. (2019). "Comparative study of silicone foam dressings versus traditional foam dressings in post-surgical wound healing." International Journal of Nursing Studies, 96, 84-92.
3. Lee, S.Y. et al. (2021). "Efficacy of silicone-based dressings in reducing hypertrophic scarring: A meta-analysis." Burns, 47(3), 530-539.
4. Williams, R.F. & Thompson, K.L. (2018). "Patient comfort and cost-effectiveness of silicone foam border dressings in chronic wound management." Wound Repair and Regeneration, 26(4), 388-395.
5. Chen, X. et al. (2022). "The role of silicone technology in advanced wound dressings: A comprehensive review." Advances in Wound Care, 11(2), 67-79.
6. Garcia-Fernandez, F.P. et al. (2019). "Prevention of pressure ulcers with silicone foam dressings: A randomized controlled trial." Journal of Wound, Ostomy and Continence Nursing, 46(2), 129-136.
_1745479303268.webp)